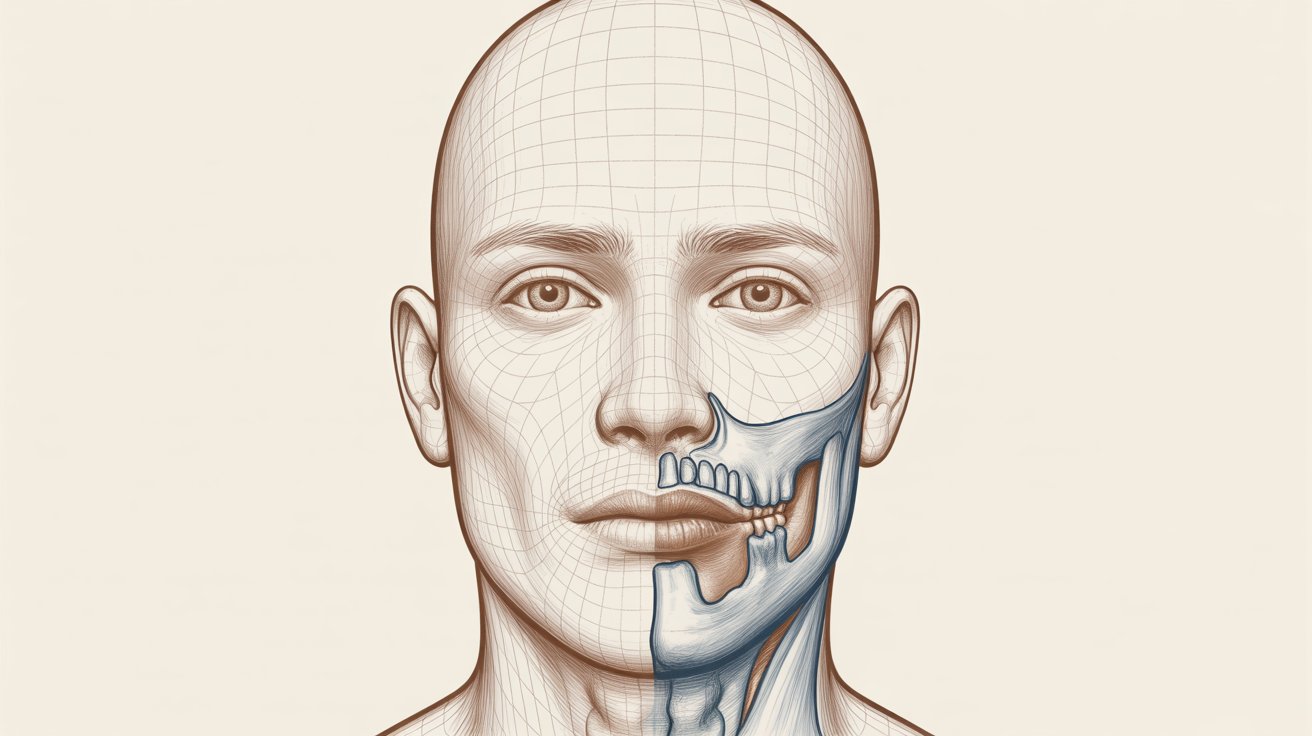
What Is TMJ Ankylosis?
TMJ ankylosis is a condition in which the jaw joint becomes stiff, severely restricted or completely fused by bone or fibrous tissue. Instead of gliding smoothly, the joint behaves like a solid block, making it difficult or impossible to open the mouth. This fusion can occur on one side of the jaw (unilateral) or on both sides (bilateral), and the severity can range from moderate limitation to complete immobility. Because the TMJ is involved in every movement of the lower jaw, ankylosis can have a profound impact on function, facial appearance and psychosocial well-being.Causes of TMJ Ankylosis
Several problems can lead to TMJ ankylosis, and understanding the cause is important for planning surgery. One of the most common triggers is trauma to the jaw joint, especially fractures in childhood that heal improperly and create abnormal bone bridges. Infections, inflammatory joint diseases and complications from previous TMJ surgery may also play a role. In some patients, systemic conditions or congenital abnormalities contribute to abnormal bone formation around the joint, gradually limiting movement until TMJ ankylosis surgery becomes the only realistic solution.Common Symptoms and Functional Limitations
The hallmark symptom of TMJ ankylosis is severely limited mouth opening, often making it difficult to eat, speak or maintain oral hygiene. Patients may also notice jaw deviation when attempting to open, chronic stiffness and discomfort around the joint area. Over time, chewing becomes inefficient, and soft or liquid diets may be adopted simply to cope with the restriction. Beyond function, facial asymmetry, changes in profile and breathing difficulties can develop, especially in growing children who rely on normal joint movement for proper facial development.When Is TMJ Ankylosis Surgery Needed?
TMJ ankylosis surgery is usually indicated when the joint is significantly fused and conservative measures cannot restore movement. If a patient can barely insert one or two fingers between the upper and lower teeth, daily functions like eating, speaking and oral care are already compromised. Progressive facial asymmetry, airway problems and pain that fails to respond to non-surgical treatments are further warning signs. In such cases, delaying TMJ ankylosis surgery can allow deformity to worsen, particularly in children, making later correction more complex.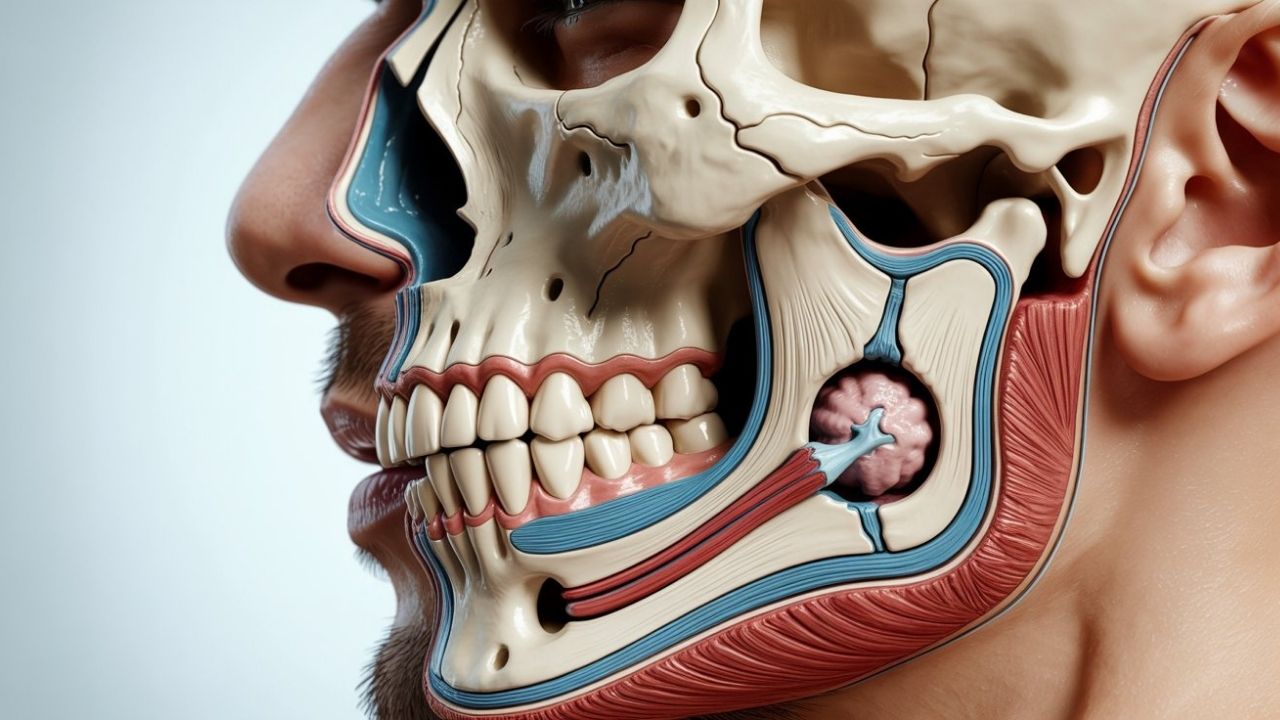
Types of TMJ Ankylosis Surgery
There is no single approach to treating ankylosis, and the choice of TMJ surgery depends on the severity of fusion, patient age, facial growth status and the presence of deformity. Surgeons assess whether the ankylosis is primarily bony, fibrous or mixed and plan the operation accordingly. In some cases, simple release of the fusion is sufficient, while in others, reconstruction or complete joint replacement is necessary. The ultimate goal of each technique is to create a stable, mobile joint that allows safe and functional jaw movement.Gap Arthroplasty
Gap arthroplasty is a procedure in which the fused bone around the TMJ is removed to create a space between the upper and lower joint components. By physically separating these structures, the surgeon prevents them from locking together again during movement. This form of TMJ ankylosis surgery is often used in moderate cases where the goal is to restore opening without complex reconstruction. Although it is technically simpler than joint replacement, careful planning and postoperative exercises are still essential to reduce the risk of re-fusion.Interpositional Arthroplasty
In interpositional arthroplasty, the surgeon not only removes the ankylosed bone but also places a barrier material between the joint surfaces. This material may be the patient’s own tissue, such as temporalis fascia or cartilage, or a carefully selected synthetic spacer. The purpose is to prevent bone from growing back across the gap and causing another episode of ankylosis. Because interpositional arthroplasty offers additional protection against recurrence, it is frequently chosen when long-term stability is a priority in TMJ ankylosis surgery.Total TMJ Joint Replacement
When the joint is severely damaged or multiple previous operations have failed, total TMJ joint replacement may be recommended. In this type of TMJ ankylosis surgery, the diseased joint surfaces are removed and replaced with a prosthetic system designed to mimic natural movement. Custom-made implants can be created based on three-dimensional imaging to match the patient’s anatomy and correct deformity. This approach not only restores mobility but also improves facial symmetry and bite function in complex cases.Combined Orthognathic and TMJ Surgery
In many long-standing cases, ankylosis has caused significant changes in jaw position and facial proportions, requiring more than just joint release. Combined orthognathic and TMJ ankylosis surgery addresses both the fused joint and the resulting skeletal imbalance. During the same surgical stage or in a planned sequence, the surgeon may reposition the upper and lower jaws to improve bite, airway and facial aesthetics. This comprehensive strategy can dramatically improve both function and appearance, especially in patients who developed ankylosis during childhood.The Critical Role of Physiotherapy After Surgery
TMJ ankylosis surgery alone is not enough to guarantee long-term success; active postoperative physiotherapy is absolutely crucial. After the joint is surgically released or reconstructed, the surrounding muscles and tissues must be retrained to support movement. Patients are typically instructed in mouth-opening exercises, stretching routines and controlled movement drills that begin soon after surgery. Without consistent physiotherapy, scar tissue or new bone may limit motion again, so long-term cooperation between patient and rehabilitation team is essential.Potential Risks and Complications
Like any major operation, TMJ ankylosis surgery carries certain risks that should be discussed openly before treatment. Possible complications include infection, excessive bleeding, injury to nearby nerves and recurrence of ankylosis if healing does not progress as planned. There may also be changes in bite or jaw position that require further adjustment or orthodontic care. Choosing a surgeon with extensive experience in TMJ surgery and following postoperative instructions carefully can significantly reduce these risks and support a more predictable outcome.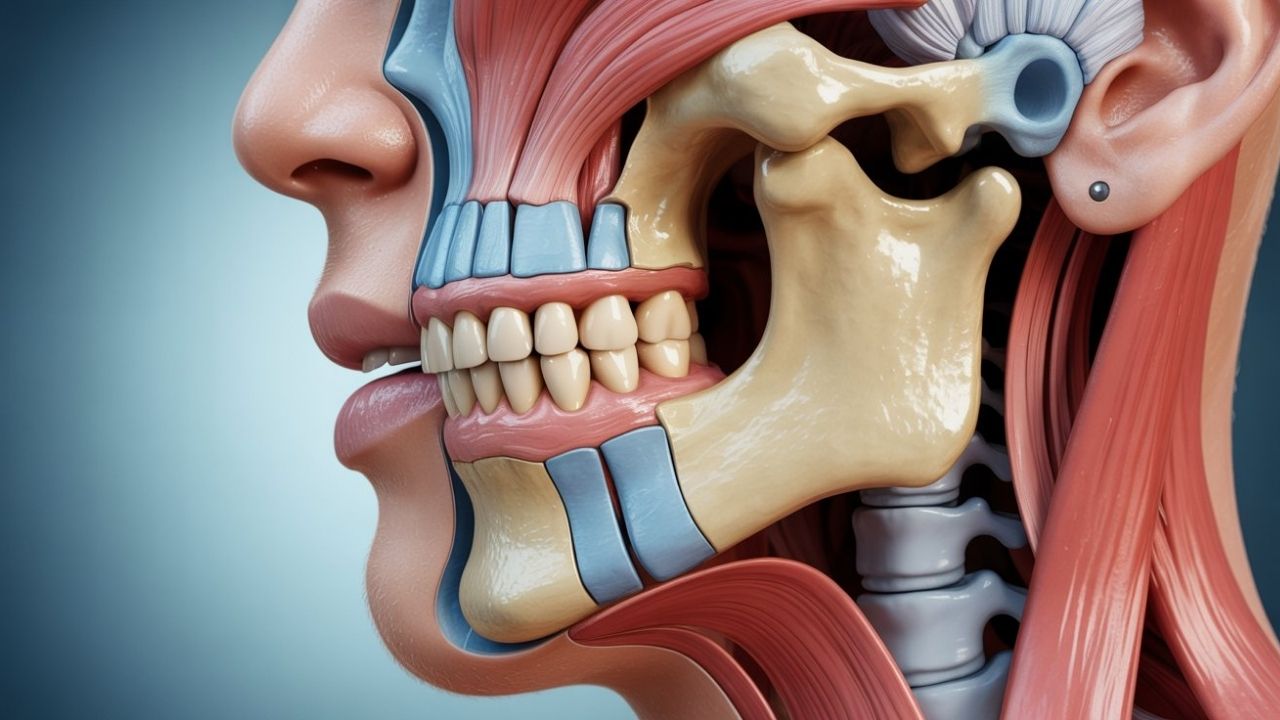
Recovery, Diet and Daily Life After TMJ Ankylosis Surgery
Recovery from TMJ ankylosis surgery is a gradual process that extends well beyond the clinic stay. In the first days and weeks, swelling, bruising and mild to moderate discomfort are common, but these symptoms typically improve with proper care and medication. Patients are often advised to follow a soft or blended diet while the joint and muscles adapt to new movement patterns. Over time, as jaw opening improves and strength returns, most people can resume normal eating and speaking activities, provided they remain consistent with physiotherapy and follow-up visits.TMJ Ankylosis Surgery in Children and Growing Patients
TMJ ankylosis in children presents unique challenges because it directly interferes with normal facial growth and airway development. If left untreated, the lower jaw may remain small and retruded, leading to breathing problems, dental crowding and pronounced facial asymmetry. Early diagnosis and timely TMJ ankylosis surgery help restore movement, support more normal growth and reduce the severity of future deformity. In some cases, staged procedures are planned as the child matures, ensuring that treatment keeps pace with ongoing development.Long-Term Results and Quality of Life
For many patients, successful TMJ ankylosis surgery leads to dramatic improvements in daily life. Being able to open the mouth more comfortably transforms simple activities like eating, brushing teeth and speaking with confidence. Reduced pain and better function can also ease social anxiety and improve emotional well-being. While long-term follow-up and occasional adjustments may be necessary, most patients experience a sustained improvement in both function and appearance, especially when they remain engaged in their rehabilitation program.