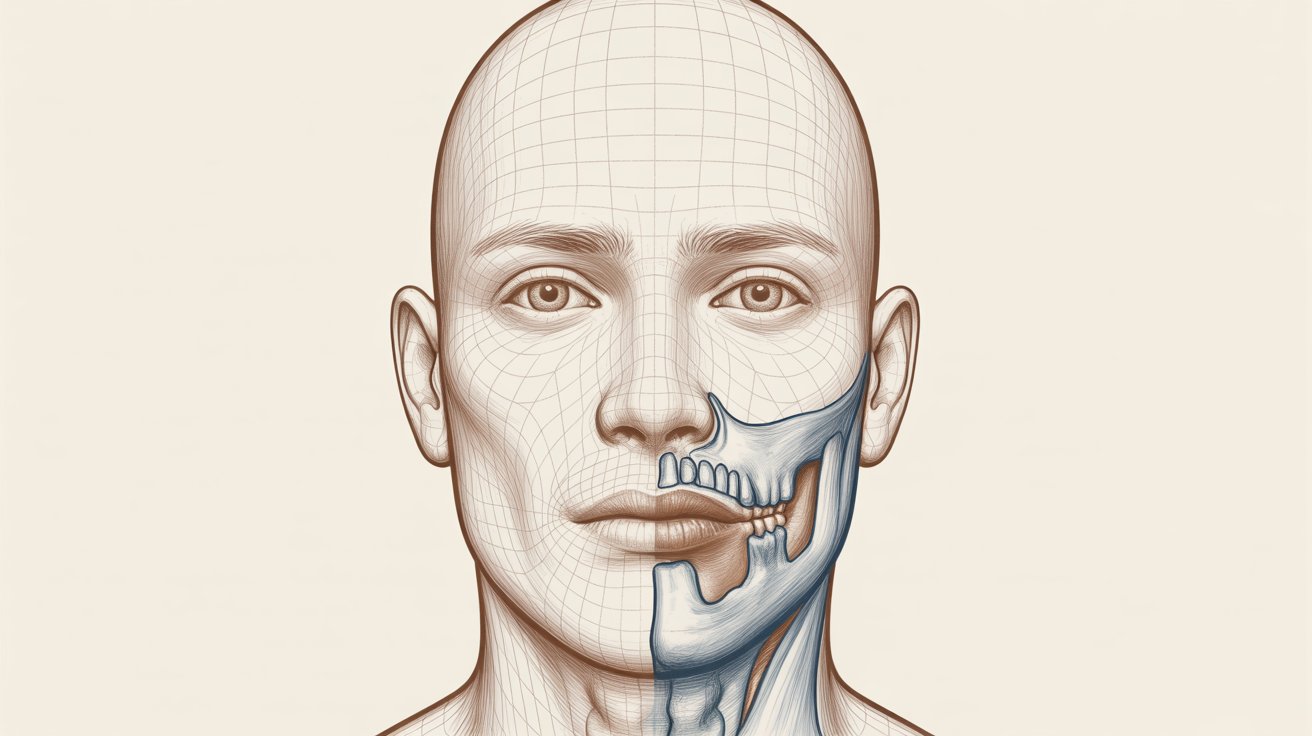
What Is TMJ Disorder?
A TMJ disorder develops when the jaw joint or the surrounding muscles fail to work smoothly. The TMJ is unique because it both hinges and slides during use, making it responsible for nearly every mouth movement. When the joint disc is displaced, the muscles become strained, or the joint itself becomes inflamed, normal function is disrupted. Many patients notice pain in the chewing muscles, stiffness, or clicking sounds when opening and closing the mouth. These symptoms may come and go, or they may gradually become more persistent over time. Anyone can develop TMJ disorder, but it is frequently linked to jaw clenching, teeth grinding, stress, trauma, or imbalance in the bite or jaw alignment.
Common Symptoms of TMJ Disorder
The signs of TMJ disorder vary widely from person to person. Some people experience mild discomfort, while others develop chronic pain that interferes with daily activities. Jaw tenderness — especially during chewing or talking — is very common. Many patients also report clicking, popping, or grinding noises in the joint, sometimes accompanied by locking or limited opening. Headaches, neck tension, ear pain, or facial soreness may also occur, as the jaw muscles work harder to compensate for dysfunction. Because these symptoms can overlap with other conditions, a detailed evaluation is essential for an accurate diagnosis.- Jaw locking or difficulty opening wide
- Uneven or uncomfortable bite sensation
- Ringing or aching in the ears
- Pain spreading to the neck or shoulders
What Causes TMJ Disorder?
There is rarely a single cause of TMJ ankylosis surgery. Instead, several contributing factors often work together. One of the most common is bruxism — unconscious clenching or grinding of the teeth — which places constant pressure on the joint and muscles. Over time, this strain leads to inflammation, fatigue, and pain. Other possible causes include trauma to the jaw, degenerative joint disease such as arthritis, misalignment of the bite, displacement of the joint disc, or stress-related muscle tension. Posture problems and underlying medical conditions may also play a role. Because the TMJ is part of a complex system of muscles and nerves, even small imbalances may eventually trigger symptoms.
How Is TMJ Disorder Diagnosed?
Diagnosis begins with a thorough medical and dental history and a careful clinical examination. Your specialist will evaluate how wide your mouth opens, whether the jaw deviates to one side, and if noises occur during movement. Tender points in the jaw muscles and joint area are also assessed. In more complex cases, imaging such as X-rays, MRI, or CT scans may be recommended to visualize the joint, surrounding bone, and soft tissues. These studies help determine whether the disc is displaced, whether arthritis is present, or if another underlying condition is contributing to symptoms.Non-Surgical Treatment Options
Most patients with TMJ disorder respond well to conservative, non-invasive treatments. Self-care strategies — such as resting the jaw, avoiding tough or chewy foods, and applying warm or cold compresses — often provide meaningful relief. Gentle jaw stretching and relaxation techniques can also ease muscle tension. Medication may be prescribed to reduce inflammation, control pain, and relax tight muscles. In some long-standing cases, low-dose antidepressants may be used to help manage chronic pain symptoms and improve sleep. Another common therapy is the use of an oral appliance or night guard. These devices reduce the damaging effects of teeth grinding and help distribute bite pressure more evenly across the jaw.
The Role of Physical Therapy
Physical therapy can be an important part of TMJ disorder management. Targeted exercises help strengthen and relax the jaw muscles, improve mobility, and enhance joint stability. Treatment may include manual therapy, posture correction, stretching techniques, and other modalities designed to relieve tension and inflammation. Patients are often taught home-care routines that support long-term improvement. Consistency is key — regular exercises and awareness of harmful habits such as jaw clenching significantly improve long-term outcomes.When Is TMJ Surgery Considered?
Surgery for TMJ disorder is generally considered only when conservative measures do not relieve symptoms or when a structural problem inside the joint requires direct repair. Minimally invasive procedures such as arthrocentesis or arthroscopy may be used to flush the joint or correct minor internal problems. In more severe cases, open-joint surgery or disc repositioning may be recommended. The goal of any TMJ surgery is to restore functional movement, reduce pain, and improve quality of life. A specialist will carefully assess whether surgery is appropriate for your situation.Lifestyle Changes and Self-Care
Many people find that small daily changes make a big difference in managing TMJ disorder. Avoiding hard, crunchy, or sticky foods can give the joint time to rest. Reducing gum chewing, correcting posture, and being mindful of teeth clenching also help relieve strain. Relaxation techniques — including deep breathing, meditation, or gentle stretching — may reduce stress-related jaw tension. Learning to maintain a natural, relaxed jaw position is another key strategy for long-term comfort.Preventing TMJ Disorder Symptoms
It is not always possible to prevent TMJ disorder entirely. However, awareness of risk factors — such as tooth grinding, stress, or poor posture — can reduce the likelihood of developing symptoms. Wearing a nightguard, taking breaks from heavy chewing, and seeking treatment early when symptoms appear are all proactive steps that support jaw health.Living with TMJ Disorder
For many people, TMJ disorder becomes manageable over time with the right combination of care, lifestyle modifications, and professional guidance. Most cases do not require surgery and respond well to conservative treatment. Working closely with your dentist or TMJ specialist ensures that your care plan is tailored to your unique needs and symptoms.